ADDRESSING HEALTH LITERACY AND OTHER BARRIERS TO COMMUNICATION
Barriers to communication
What patient characteristics might represent a barrier to communication, either in face to face consultations or in remote consultations, by telephone or video?
Hover on the icons below to find out more.
Question
Which of these barriers might be hidden?
please select one of the following
Question
Can you think of any strategies to address these barriers to communication?
Consultation recall
Even if no obvious communication barriers are present, memory is an issue for almost all consultations.
Question
How much of the consultation do you think that patients typically remember?
Recall of the consultation is not linked to age, or intelligence but may be associated with health literacy.
Importantly, people may have good literacy in other areas (e.g. related to their occupation) but have poor health literacy.
Limited recall of the consultation is associated with lower adherence to recommended treatment.
Amount of recall can be enhanced by:
Using shorter sentences
Giving information in chunks
Checking
understanding
These are all techniques for addressing health literacy, some of which are detailed below.
Health literacy
Health literacy is about accessing, understanding and using information to make decisions about your health. It’s a balance between individual characteristics, like skills and motivation, and the complexity of the health care environment or materials.
Health literacy encompasses a number of different skills, including:
Reading
Listening
Speaking
Interacting
Critical thinking
Comprehension
Numeracy
Importantly, people may have good literacy in other areas (e.g. related to their occupation) but have poor health literacy.
This will make it difficult to know who has poor health literacy.
Why Health literacy is important
Impaired health literacy is common. In England, 2 in 5 adults aged 16-65 struggle to understand textual health information materials.
The average reading age in the UK is 9. Here is an example of two sentences about osteoporosis.
Click on each sentence to reveal the reading age.
Click on the boxes to find out more:
This sentence has a reading age of 16/17.
This sentence is too complex for the average UK adult with a reading age of 9-11
Reading age 9/10
If numbers are included within text, then 3 in 5 adults of working age find it hard to understand the information. These numbers are likely to be higher for older populations.
Limited health literacy is linked with unhealthy lifestyle behaviours such as poor diet, smoking and a lack of physical activity. Having impaired health literacy is a risk factor for lots of poor health outcomes.
Increased risk of being admitted or attending A and E
More frequent and longer hospital stays
Less likely to adhere to prescribed or recommended treatments
Increased risk of depression and developing multiple health problems
Higher mortality rates
How to address health literacy and what techniques to use
It is not easy or possible to identify people who have low heath literacy. For this reason, experts recommend clinicians adopt ‘universal precautions’. This means adopting techniques for communicating with people with low health literacy in every consultation. Universal precautions for health literacy in verbal communication involves:
Encourage questions
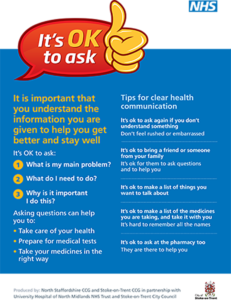
To learn more about how you can promote question asking, click here for information about Stoke-on-Trent’s ‘OK to Ask’ campaign.
Teach-back
To enhance and check understanding you can use a technique called ‘teach-back’
Often we check understanding using questions like – ‘does that make sense?’ or ‘Have you understood everything?’
These sort of questions are not very effective because
- They beg a yes/no answer, so even if the patient answers ‘yes’ we don’t really know if they understand
- The patient may feel put on the spot and as if they are being tested and may not want to admit they do not actually know, or only partially understand
- The patient may think they understand, but may not have grasped all the relevant information
‘Teach-back’ is a method of checking understanding where you ask the patient to explain back to you the information that has been shared.
Questions may include:
- “I would like to check that I have explained things properly, would you mind telling me what it is we have discussed and what we have agreed you will do?”
- “Can you tell me how you are going to explain things to your family when you get home tonight?”
These sort of questions are effective because
- The onus is on checking the health professional has explained properly rather than testing the patient.
- The technique enables the health professional to check that they have clearly explained information in a way that the patient understands.
The use of the teach-back technique has been shown to improve outcomes such as
- understanding
- satisfaction
- health outcomes such as adherence to medicine
This very short video gives a couple of other examples of how Teach Back can be used
This video gives an example of Teach-back in an iFraP consultation:
Involving wider family and/or friends
Involving the patient’s wider family, friends and/or carers can be helpful to address these barriers.
We can do this through
- Providing understandable written information the patient can share with family, friends and/or carers before, and after, the consultation
- Involving a ‘medical visit companion’ in the consultation
A research study of more than 12,000 people aged 65 and over who were seeing their doctor found that the people who were accompanied were more likely to be engaged in communication, were more satisfied and rated the information giving higher.
A consultation companion can help communication by
- Providing information
- Asking questions
- Explaining clinician instructions
It’s therefore important, if the patient is accompanied, to involve the companion in the discussion. If we’re talking to people on the phone, we can ask who else is there, and if speakerphone can be used (if the patient consents to someone else participating) to aid the communication.
You have now completed this section
Click below to move to Communicating risk