The iFraP consultation
Overview
There are 8 steps to the Fracture Liaison Service consultation
1. Greeting / Introduction
Explain the aim of the appointment and find out what the patient is expecting from the appointment.
We covered the importance of this in Shared Decision Making.
2. Gathering information
- Take a history, including information about the fracture, medical history, fracture risk factors, falls and lifestyle behaviour
- Recommend, arrange and explain tests including DXA, spinal imaging and blood tests if appropriate
Depending on the service model in your FLS, and whether your clinics are ‘one-stop shops’ you may or may not gather information in the same consultation as you discuss management with the patient. We have not covered gathering information in this training. Speak with your line manager or trainer if you have concerns about this aspect of the consultation.
The iFraP tool is designed to support you with the following aspects of the consultation:
3. Considering therapeutic options
Use national guidelines to decide which patients should be offered a drug.
4. Eliciting patient perceptions
Ask the patient what they already know and think about osteoporosis, osteoporosis medicines and their concerns and how important maintaining independence is.
5. Establishing Shared Decision Making preferences
Establish what involvement the patient would like to have in making decisions about medicines.
6. Sharing information about the condition
Show and explain bone density results.
Explain, building on what the patient already knows
- what osteoporosis is
- the causes
- the consequences
- how it can be controlled
7. Sharing information about treatment
Discuss the role of lifestyle management, including, as appropriate:
- diet and supplements,
- physical activity,
- avoiding falls,
- smoking cessation
- alcohol reduction
Discuss drug treatment including explanation of:
- why the treatment is recommended,
- aims and benefits,
- common or severe side effects,
- what is involved in taking the medicine
- how long it will be taken for
- How effectiveness is monitored
8. Checking understanding and summarise
- Check patient understanding and ask about any concerns
- Ask if the patient is willing to take the recommended option, prefers not to take it or if they are still unsure
Tips on using the computer in the consultation
Some people worry about the computer detracting from the patient-clinician relationship.
Did you know that using a computer in the consultation has actually been shown to reduce the distance between patient and clinician and increase patient satisfaction?
Picture from research by Almquist et al
Hover over the dots in the picture below to find out more about how to use the computer in the consultation
Ensure the room is laid out in such a way so that the patient can see the screen without turning or twisting, and you can easily move from looking at the computer, to the patient
Ensure the iFraP tool is open before the patient enters the room
Explore and negotiate the patient’s agenda before using the computer
Move the computer’s screen to offer the patient a visual access to the screen
Keep a position facing the patient most of the time with hands away from the keyboard
Indicate when the computer is used and explain what is done
Indicate to the patient where your attention is directed on the screen by using verbal and non-verbal clues
Invite the patient to consult the information displayed on the screen
Give full attention to the patient by not looking at the computer when he/she expresses emotions or psychosocial issues
Using the iFraP tool face to face
Clinician treatment decision support
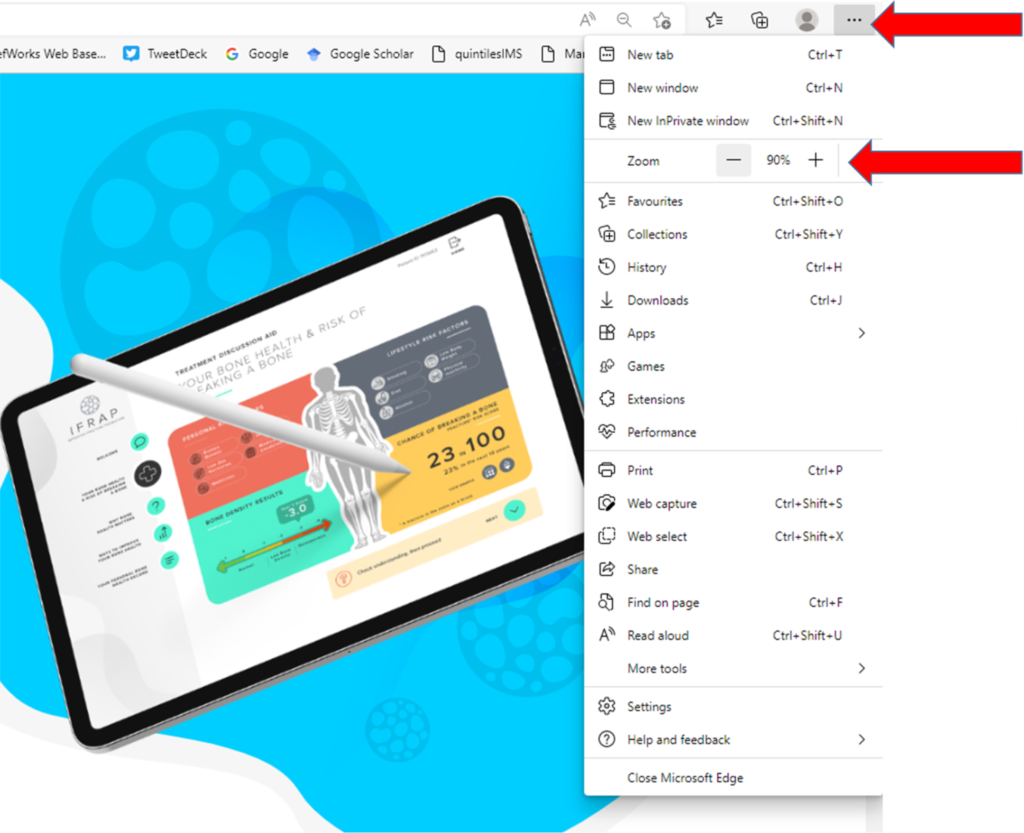
Enter your username to gain access the tool. If the display is too small or large for your screen you can change the size using the 3 dots at the top right of your screen.
After entering basic patient clinical information, the tool will suggest treatment options. You can then further refine or change the list to choose which drug option(s) to present to the patient in the treatment discussion aid.
Note that when the tool refers to oral bisphosphonates this covers alendronate and risedronate
*It is important not to use the back button when navigating through the tool.*
Watch this brief video which explains this section of the iFraP tool
TREATMENT DISCUSSION AID
The treatment discussion aid is split into the following sections:
- Why bone health matters
- Your bone health and risk of breaking a bone
- Ways to improve your bone health
- Your personal bone health record.
Each of these sections will be discussed in turn.
Why bone health matters
Before giving information to the patient, watch out for the reminders to ask patient what their thoughts are.
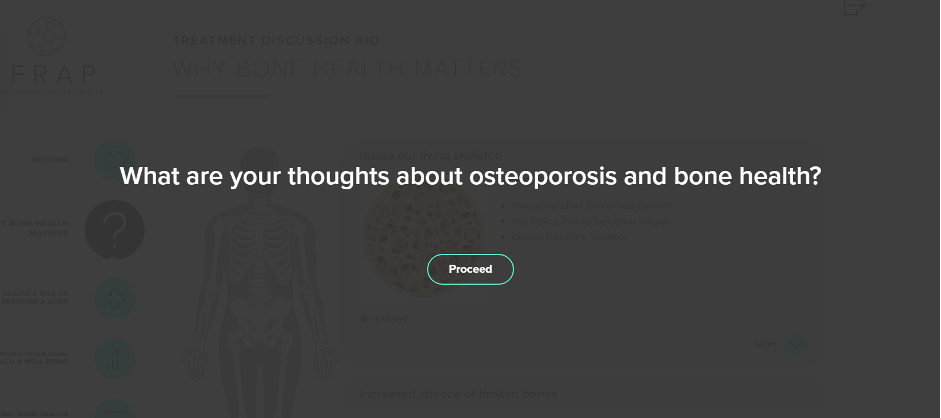
If the patient has osteoporosis, remember to find out what they already know about it, to fill gaps in their knowledge.
Explain what happens inside the bone (animation available), what this means in terms of fractures and what the consequences of fractures might be, particularly in the spine (animation available).
Watch this brief video which explains this section of the iFraP tool
Your bone health and risk of breaking a bone
Explain that bone strength is affected by a number of things. If the patient has already broken one bone, we know this puts them more at risk of breaking another. They may have other risk factors. If we have measured bone density we can explain it here. Their T score will be displayed with an arrow pointing to a scale of BMD to display whether the T score falls into the range of osteoporosis. We can say that we use all this information to estimate their risk of breaking a bone. When explaining their risk, you can flag that you are shortly going to show how this can be reduced. Remember to check understanding.
Watch this brief video which explains this section of the iFraP tool
Ways to improve your bone health and well-being
In this section, ask the patient what aspects of management they would like to discuss. You can click on lifestyle buttons for more information if you or the patient want to. The tool flows better if lifestyle management is discussed before medicines.
The medicine section includes 3 aspects
- why this medicine is important
- possible side effects
- practical issues
Throughout the tool you will see this icon to remind you to check understanding and use TeachBack if appropriate.
Watch this brief video which explains this section of the iFraP tool
Your personal bone health record
The final page of the tool sums up the discussion about medicine, and the patient views. In this section you ask the patient some questions and complete them on the tool. The answers to these questions will filter through to the printed bone health record.
The purpose of these questions/the bone health record is to
- Increase patients’ commitment to medicine and help the patient remember about the need for treatment
- Help the GP or primary care practitioner by demonstrating what is important to the patient.
- Help the patient have ongoing conversations about their condition and treatment.
The bone health record can also be completed for patients who do not receive a drug recommendation.
The bottom of the Bone Health Record contains a QR code/URL for a page on the iFraP website. Patients will have access to a ‘your Bone Health Record explained’ video. This video will include the full demo of the iFraP tool including the animations in Your Bone Health and Why Bone health matters. This means that patients who have a telephone consult can still see aspects of the tool after the consultation, and patients who have had a face to face consultation can also effectively view the tool again (although the explanation will not be personalised to them).
what patients in iFraP said about the Bone Health Record
"Me and my GP should both be singing from the same hymn sheet"
Patient 1
“My boss was very concerned that there were going to be other issues as well, so I think this bone health record will alleviate her concerns as well because I'll share it with her.”
Patient 2
Watch this brief video which explains this section of the iFraP tool
Closing the consultation
- Arrange and explain follow-up for patients, including when they are unsure about treatment and offer helpline to discuss further
- Offer advice and onward referral for fracture management and/or falls prevention if appropriate
- Give the patient contact details and written information
- The bone health record which details the key information from the tool for the patient should be completed. After you click on ‘next’ at the bottom you can then print or save the record. The record should then be given to the patient during the appointment or posted and/or emailed afterwards.
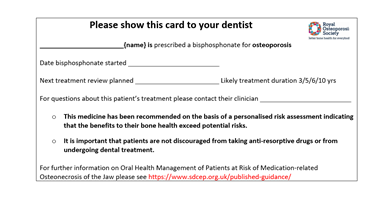
- A treatment card to share with their dentist. This explains to the dentist why treatment is needed.
- Signpost to the Royal Osteoporosis Society website, where there is further information
- Ask what questions the patient has
- Include a copy of the bone health record in the correspondence to the GP, so they have the same information about risks benefits and harms.
Consultation demo videos
Here is an example consultation using the iFraP tool.
In the next section, there follows some advice on how to adapt the conversation for different circumstances.
In a face to face, one stop clinic
The tool can be open during the clinic. After the greeting and gathering information, enter clinical information into the tool and proceed to use the tool during the rest of the discussion. The patient can be handed, and the GP sent the PDF output after the consultation.
In a face to face appointment to discuss treatment
Clinical information can either be entered into the tool just before the appointment) or at the start of the consultation. Proceed to use the tool during the rest of the discussion. The patient and GP should be sent the PDF output after the consultation, electronically or by mail.
In a patient in whom medicines are not recommended
The tool can still be used to explain bone health results (fracture risk), BMD results and lifestyle management. One FLS clinician we spoke to highlighted the importance of using the tool in Fracture Liaison Service appointments, even if the patient did not have osteoporosis:
One clinician said: “we’re not just here to treat patients with osteoporosis, we’re here to prevent it as well that’s the ethics really of the service to reduce the risk of fracture and prevent them developing osteoporosis.”
See the example clip of a consultation where no drugs are recommended
In a telephone clinic to discuss medicines
Clinical information can either be entered into the tool just before the appointment or during the consultation.
You can use the tool to guide your discussion. The patient and GP should be sent the PDF output after the consultation.
The bottom of the Bone Health Record contains a QR code/URL for a page on the iFraP website. Patients will have access to a ‘your Bone Health Record explained’ video. This video will include screens on the tool including the animations in Your Bone Health and Why Bone health matters. This means that patients who have a telephone consult can still access aspects of the tool after the consultation.
See the example clip of a telephone consultation
Where two drugs are discussed
If you select more than one drug an additional screen will show a side by side comparison of the drugs. It is worth noting that the treatment benefits are similar for a number of different drugs where you might expect one drug (e.g. romosozumab) to be superior. The ‘ticks’ are based on best available evidence but are also fairly crude so will not illustrate small differences in efficacy between drugs.
See the example clip of where more than one drug is discussed
Where the patient is not keen on medicine
If the patient is not keen on medicine we must respect their decision. We can still explain it is helpful to give them all the information in case they change their mind or to inform there decision/discussion with family and friends. It is worth while considering what your response will be if they need more time (will you offer a follow up?) if you are not used to asking patients if they are willing to take medicine or not.
See the example clip of completing the bone health record with someone who is not keen on medicine
Where the patient will be referred on to discuss intravenous treatment
If the patient is going to be referred on to another clinic it is still helpful to give them a brief overview of the medicine so they know what to expect.
See the example clip of how to use the tool with someone who will be referred on
Where the patient is already taking an osteoporosis medicine
If your patient is already taking osteoporosis medicine it is still helpful to go over the basics as most patients will not have had a complete explanation of treatment benefits, harms etc when medicine is started. This may increase their commitment to medicine in the long term. As always, aim to fill in the gaps in patient knowledge with your explanation.
See the example clip of using the tool with someone already prescribed alendronate
Osteoporosis follow up consultations
Follow up consultations are an opportunity to support informed adherence. The bone health record can be retrieved. Use the information to reiterate what benefits the patient thought was important and/or to pick up on any concerns the patient had in the last consultation.
Ask about
- Any difficulties with the medicine
- Unanswered questions
Reiterate (using the bone health record)
- Benefits the patient thought was important
- Expectations for treatment (working silently in background)
- Long term plan, including the importance of long-term treatment
You have now completed this section
Click below to move to Summary/next steps
