WELCOME AND OVERVIEW
Introduction
Welcome to the iFraP consultation skills course. This course is designed to help you further develop your skills for communicating effectively with patients about osteoporosis and the potential harms and benefits of osteoporosis drug treatment options.
The course consists of five parts and will take you approximately 3 hours to complete. We recommend that you find an opportunity to complete this eLearning course with limited distractions.
This course has been developed by Dr Zoe Paskins, Dr Laurna Bullock, Prof Janet Lefroy, Prof Sarah Ryan, Prof Jo Protheroe and Sarah Leyland and is approved by the Royal Osteoporosis Society.

The patient and clinician quotes used are based on stories from Keele’s Research User Group, the Royal Osteoporosis Society patient advocate group and from the qualitative research conducted in iFraP. We have changed people’s names.
Learning outcomes
This course is about person-centred care, shared decision making, health literacy, risk communication and how to use the iFraP tool. We know that you will already be using a shared decision making and person-centred approach but hope this course will enable you to further enhance your skills.
BY THE END OF THIS COURSE YOU WILL BE ABLE TO:
-
Understand the relationship between communication skills and drug treatment uptake
-
Explain what shared decision making is and why it is important
-
Describe key skills to facilitate shared decision making
-
Explain what health literacy is and why is important
-
Understand how to take ‘universal precautions’ for health literacy
-
Understand how to communicate risk
-
Understand how to give a diagnosis of osteoporosis, and use optimal language for describing osteoporosis and osteoporosis drug treatment
-
Understand why and how the iFraP decision support tool was developed
-
Understand how to use the iFraP decision support tool in consultations
How to use this e-learning course
This course is designed to enhance your communication skills. Some elements may already be familiar to you. This course contains a mix of text, videos, pictures and mini-quizzes. You should have already completed a pre-course quiz (by email) and there is a link to a post course quiz which will take you to a separate link in Microsoft forms. Please include your email address so we can send you a certificate of completion.
PLEASE NOTE
-
The references to further information and scientific evidence which supports the e-learning are available in hyperlinks throughout the course and listed at the end.
-
The e-learning is best completed on a desktop, laptop and tablet (in landscape mode) - The e-learning course is not available on mobile
-
The e-learning does not save your progress so please remember your section if you are not completing this in one sitting.
-
Throughout the e-learning there are questions for you to answer – these are highlighted in yellow
-
Even if you feel you are familiar with the content, it is really important to complete all the sections
What is iFraP trying to acheive?
The iFraP study is developing resources to support communication about osteoporosis and its drug treatment in consultations.
The aim is to use a person-centred approach to address barriers to osteoporosis treatment uptake.
iFraP resources and training
Enhanced communication
Person-centred approach
Improved outcomes including medicine uptake
PERSON CENTRED CARE
Being person-centred is about focusing care on the needs of individual. Ensuring that people’s preferences, needs and values guide clinical decisions, and providing care that is respectful of and responsive to them.
Watch this short video to find out more
BARRIERS TO OSTEOPOROSIS TREATMENT UPTAKE
Many people with osteoporosis do not start, or, continue taking recommended osteoporosis medicines. Studies have shown that 1 in 4 people recommended an osteoporosis medicine do not start it, and less than 1 in 2 people keep taking osteoporosis treatment for more than 1 year.
One of the patients we interviewed in our iFraP development study decided not to take Alendronate. She said:
The side effects outweigh the goodness that it does because I still don’t know what it does (…) I think if those avenues were explored and mentioned and I could have told them any fears that I had, that may have helped me to decide
Patient
Let’s look at some of the reasons people do not take osteoporosis medicines
Click on the boxes to find out more:
“I am healthy enough”
“I don’t believe I am at ‘risk’”
“I don’t believe I have osteoporosis”
“It’s just normal for age”
“I am worried about the side effects”
“I don’t trust medicines”
“My friend/dentist/GP said it was dangerous”
”I am not sure I’ll remember”
”It’s a bit complicated”
”It interferes with the way I take my other medicine”
”I don’t think that the medicine is making any difference”
”I don’t feel well when I take it”
Question
What do you think would make people more likely to engage with recommended treatment plans?
Using a person-centred approach to overcome barriers to treatment uptake
Using the principles of person-centred care and shared decision making, helps us to help patients to make the best decisions for themselves. It helps us to understand the patient’s situation and beliefs, understand their preferences, priorities, and concerns, and talk about options.
To maximise the chance that any information we share is understood, and remembered, you can use techniques to address health literacy and ensure we communicate risk in the optimal way.
FLS clinicians we have spoken to told us risk communication was something they wanted extra training in.

Decision aids are tools designed to facilitate shared decision making, patient involvement and to aid risk communication.
A large Cochrane Review identified that using decision aids ;
-
Improves patient involvement and patient knowledge
-
Reduces decisional conflict (meaning patients are more sure they have made the right choice)
-
Improves the uptake of preventative medicines
Also, another large systematic review found that using a decision aid in the consultation did not increase the time taken in the consultation.
Using these approaches can help us overcome barriers to treatment uptake, particularly if lack of engagement is based on misinformation or beliefs which we might consider as incorrect. However, not everyone will want to take medicine that is recommended and people are entitled to make their own choices and decisions.
iFraP resources
IFraP has been designed to take these issues into account and includes:
Click on the boxes to find out more:
A training package – which includes this e-learning course and face to face workshop. These address enhanced communication skills relevant to shared decision making and increasing patient understanding.
The iFraP decision support tool
The iFraP decision support tool should be used on the computer during FLS consultations. The tool includes 2 parts.
- Clinician decision support, to support clinicians to know which patients, according to national guidelines, should be recommended drug treatment.
- A treatment discussion aid to support the discussion between the patient and clinician about medicines.
More information about the iFraP decision support tool is provided below
- The iFraP personal Bone Health Record. This is a print-out at the end of the tool containing a key summary of the patient results, recommendations and the patient’s thoughts and next steps.
- Patient pre-consultation letter explaining what a Fracture Liaison Service is and why bone health is important
- Patient website including a video of the tool being used and with videos and more information about the iFraP tool, how it works and how it was developed
- Patient dentist cards, with information about the patient’s bisphosphonate for patients to share with their dentist
You can find these resources on the website.
The iFraP personal bone health record however is not included, as this is printed from the iFraP tool, individualised to each patient.
iFRAP DECISION SUPPORT TOOL
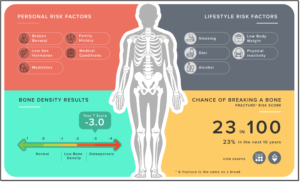
The decision support tool consists of two sections. The first section consists of clinician decision support, to support clinicians to know which patients, according to national guidelines, should be recommended drug treatment.
The second section is designed to support the discussion between the patient and clinician about medicines. This part is called a treatment discussion aid. This is similar to a decision aid.
Watch the video for a brief overview of the iFraP tool.
We will explain in more detail how to use the tool in The iFraP Consultation section. The link to the tool is also in the website so please take a look.
HOW iFRAP WAS DEVELOPED
The iFraP tool has been developed with patients and clinicians and experts in shared decision making, health literacy and medicines adherence.
The scientific information was agreed with external scientific experts (Dr Nicky Peel, Chair of the Clinical and Scientific Committee, Royal Osteoporosis Society, Professor Stuart Ralston, Chair of Osteoporosis SIGN guidance and Prof Celia Gregson, Chair of National Osteoporosis Guideline Groups).
To find out more, Professor Rob Horne, who is an expert in medicines adherence, explains in this video how iFraP has been informed by behavioural medicine and theories of medicine adherence.
HOW iFRAP has been tested so far
We have tested iFraP in one site. Clinicians and patients were really positive about the difference it made.
One clinician, after using the iFraP tool in their consultation, thought that use of the tool helped to increase patient involvement in the consultation:
“I think it involves the patient more and I also felt it makes me really feel more at ease with the patient because you’re kind of involving the patient and you’re getting to know the patient just a little bit more”
CLINICIAN
One patient reflected on their consultation where iFraP was used:
“He asked me questions and then supported it with things on the computer. It just felt more balanced and also there were no issues with answering questions because he answered the questions that I had. It just felt more of a conversation consultation rather than giving information which was quite nice.”
PATIENT
Another patient reflected on how use of the tool helped them to make a decision about medicines that was right for them:
“Everything tells me that I should be taking it. I think when you reflect back to the very first slide of the tool with the T-score, I could see that I was the lower end and that made it more sensible to take the medication. You go from the first slide to the last slide and it does make it a little bit more understandable as to why you should take it because you're that low in the score.”
PATIENT
Another patient reflected on how iFraP changed their preconceptions relating to side effects:
“Obviously, there are side effects and I'd heard there was a lot of side effects on these Facebook pages. However, when she went through the numbers on the iFraP tool of how many people did get this and that, I found that was more beneficial and it kind of shot those people on Facebook out of the water”
PATIENT
You have now completed this section
Click below to move to shared decision making
